Very interesting this article in the section Cuídate del diario Marca, in which the Cardiologist Pablo García García explains us what the Stents are and their use.
Vulgarly called springs, stents are tiny metal prostheses designed primarily to treat the lesions that atherosclerosis produces in the vessels that nourish our heart muscle: the coronary arteries.
Since their introduction at the end of the 1980s, they have evolved and improved their performance, with around 100,000 of these devices being implanted in Spain each year.
What does a stent look like?
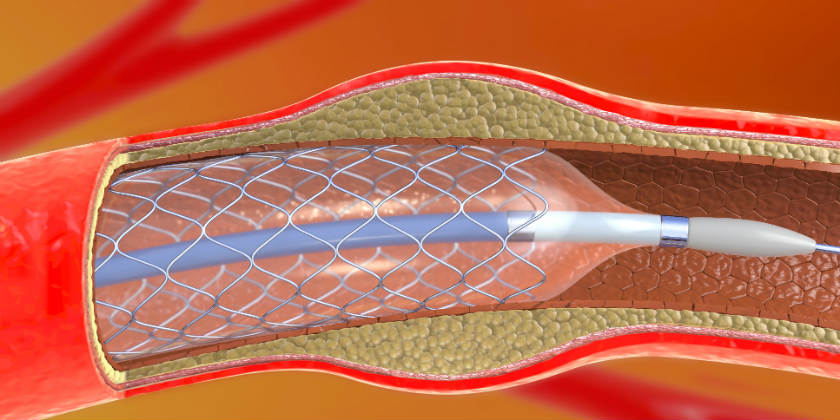
A stent is like a metal mesh that is placed in the artery by inflating a small balloon, called an angioplasty balloon.
Watch the back of your hand for a moment. You’ll see a few superficial veins. These run through the coronary arteries to the surface of your heart to provide it with oxygen and nutrients. But they’re half as thick, so a stent is effectively very small, a few millimeters wide when it’s expanded.
The first ones were made of stainless steel, then new metal alloys have emerged (cobalt chrome or platinum chrome), and finally even non-metallic stents that are absorbed and disappear after 2-3 years.
This tiny piece of engineering is like a metal mesh, designed to stick to the innermost wall of the coronary artery and expand areas of narrowing, improving blood flow.
How do they work?
The stent travels to its destination folded over an angioplasty catheter. It is accessed through a puncture in the skin. Usually in the radial artery, where we take the pulse in the wrist and the path to the heart is guided by x-rays.
To release it, a small balloon, called an angioplasty balloon, is inflated. This is done at great pressure to get the stent to adhere completely to the coronary wall. Ultimately, the stent works in a manner similar to a form, causing the coronary vessel to regain its caliber.
The most commonly used stents are those that are coated with drugs. This prevents the internal wall of the vessel, which is a living tissue, from causing a rejection reaction. This may cause the artery to re-narrow, which is known as restenosis.
Where are they used?
Stents are used to treat atherosclerotic disease, which is a deposit of cholesterol that can occlude our coronary arteries by reducing their size. This process can be progressive, generally linked to ageing and cardiovascular risk factors (diabetes, hypertension, hypercholesterolemia, smoking, renal failure).
However, it can also be an abrupt process, because if these cholesterol plaques break, blood flow can be rapidly interrupted. If the flow is completely interrupted it is known as acute myocardial infarction; if it is incomplete it is called unstable angina.
It is precisely in these situations that this procedure is most useful, since in a short period of time blood flow can be restored. A stent is implanted over the area that has broken and produced the narrowing to prevent it from occluding again.
This technique is more accessible than restoring coronary flow through heart surgery, so it is the treatment of choice in acute attacks.
When is bypass surgery preferable?
In situations where time is of the essence, such as acute myocardial infarctions, it is faster to perform a catheterization and use stents to unblock the affected coronary artery. This allows the heart to receive blood supply again as soon as possible and decreases the damage that will remain.
The surgery restores blood flow by using shunts, which are bridges made with grafts of veins or arteries, to bypass the blockage. This technique has the advantage of being more durable in the long term. On the other hand, it involves more time and is more aggressive for the patient.
Surgery is usually the best option when we have coronary disease affecting the three coronary arteries, the left common trunk and in diabetics, because they usually have more diffuse coronary involvement.
The decision about the best option of the two corresponds to what is known as the Heart Team. It is a team made up of cardiologists, surgeons, interventional cardiologists and anesthesiologists, among others, who agree on the best option for each case. Sometimes, even though the ideal option is surgery, it may be ruled out because the risk is too high. This often happens in older patients and with other diseases that increase the risk of surgery.
In addition, if the coronary disease progresses over the years, stents may be implanted in patients who have undergone surgery. Similarly, if a patient has not done well with stent implantation, surgery can be considered later, as they are compatible techniques.
Therefore, surgeons and cardiologists work closely together because each patient is a unique case and will need one technique or another or, as we have seen, different types of intervention throughout their lives.
Why do I have to take two antiplatelet medicines?
When the first stents were implanted it was seen that the artery could become suddenly occluded again, which is known as stent thrombosis. This complication was reduced by high-pressure inflation, but it was mainly due to the generalization of double antiaggregate therapy.
The double antiaggregate therapy involves taking, in addition to aspirin, which is an antiplatelet agent, another medication (usually clopidogrel, prasugrel or ticagrelor) to prevent platelets from forming aggregates on the stents.
Patients usually take these two drugs together for about 6 to 12 months. These times are increased in some cases, but also shortened when necessary. For example, when the patient is going to undergo a surgical intervention or procedure with a high risk of bleeding, since logically taking these medicines the risk of bleeding is greater.
Conclusions
Since their implantation, stents have been a revolution in cardiology because they allow faster and more effective treatment of acute heart attacks.
Coronary artery bypass surgery is more effective and durable in the long term and is indicated in certain situations, but usually not in emergencies.
Stent implantation necessarily involves the combined treatment of two anti-aggregation drugs over a period of time and this must be taken into account.
* Clinical cardiologist at Don Benito Villanueva Hospital (Badajoz).
Congratulations to the newspaper Marca for this great information, the original news in Diario Marca
Complete information thanks to Dr. Pablo García García
In Málaga centrocardiovascular.es for the care of your cardiovascular health. Cardiovascular Center Dr Aranda.